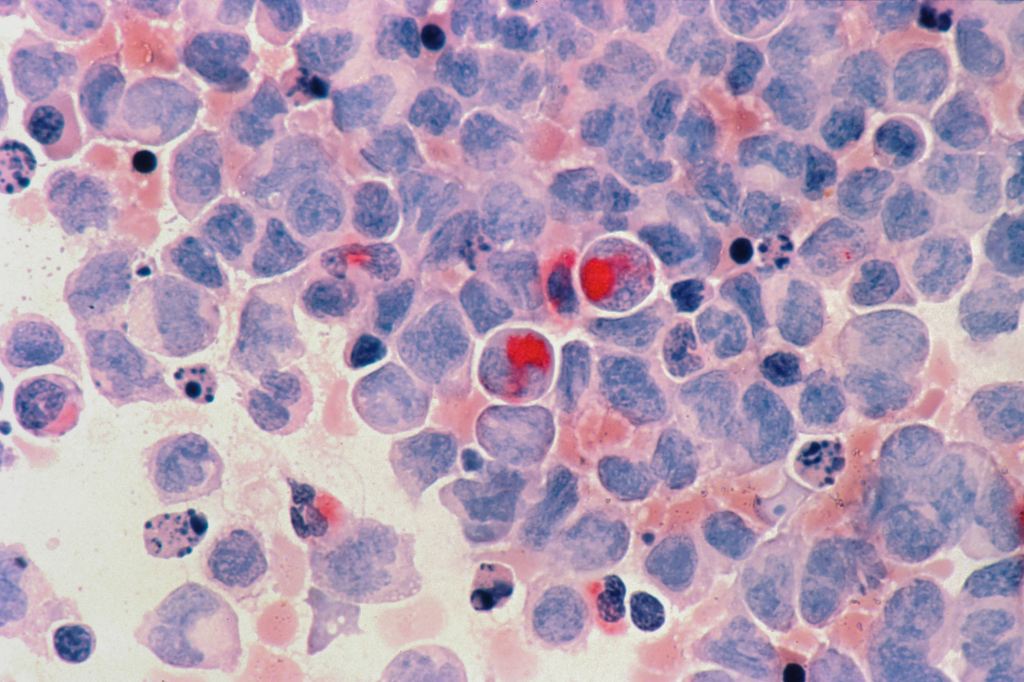
We tailor the information we give to the needs of the people we are dealing with. Everyone is different. Some will need to know as much as they can. Others will only want to know the bare minimum. Some can only listen to the positive aspects of the information. We try not to extinguish hope, but one thing that is certain in life is death. Sometimes we may have to reframe hope and even miracles. We hope that you will be kept comfortable. It will be a miracle for you to not be in pain or distress. It can be hard for people to stop having tests done. They may have had regular blood tests for many months or years in some cases. Following disease activity markers as if they were fluctuations in share prices, but with much more at stake than money.
Not everyone can accept what is going on. We will try our best to prepare people for impending deterioration and death. We want to try to prevent complicated grief if at all possible. There is no escaping the fact that a person will be dying soon. How long have they got left? We often say we don’t know. We will try to give our best estimate or our best-educated guess. We cannot predict what will happen. We try to anticipate what happens commonly. Each individual situation can be different from what is expected.
We can’t make anyone accept that they or their loved one is dying. The brain might be able to understand and accept what is going on, but the emotional heart takes a lot longer. There will be some people who will never be able to accept what is going on. For these folk, we might need to go into damage-control mode. We wish we had better news to pass on. We can only try to prepare people but sometimes we will not be successful. Some cases will be rough. We must stay calm and all tell the same story.