When it comes to being told stuff do you want to know the full details?
Nod.
My colleague said that you want us to be straight up with you, is that right?
Nod.
What did the doctors at the hospital tell you?
They said it was pretty bad.
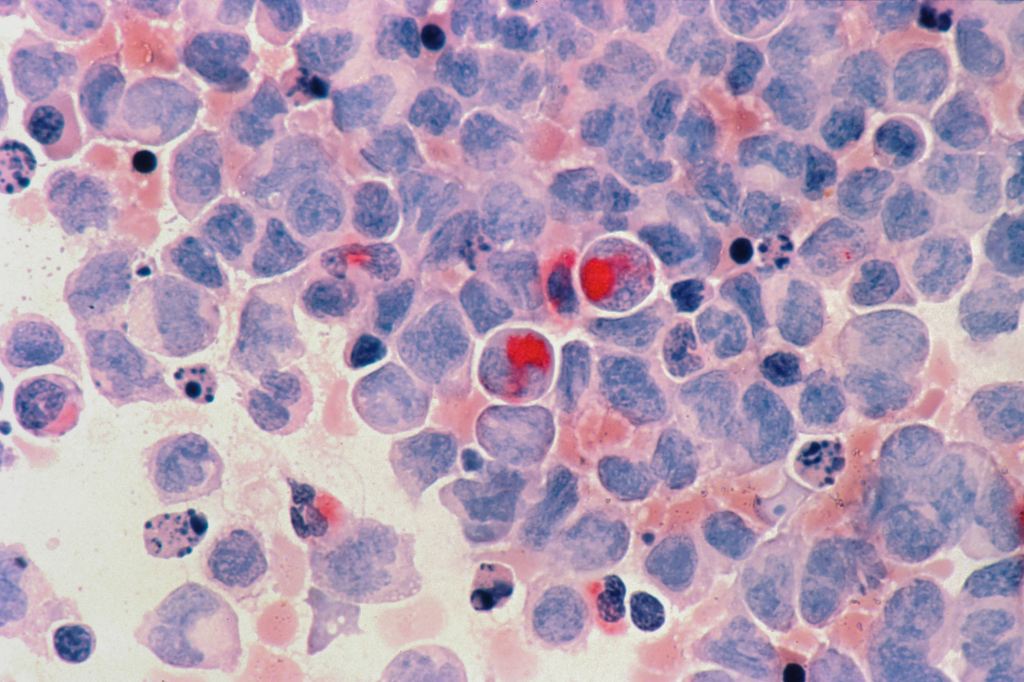
Yeah. What happens with Leukaemia is that one type of abnormal blood cell takes over the bone marrow. The bone marrow is your body’s factory, it makes all the blood cells. The red blood cells carry oxygen around. The white blood cells fight infection and the platelets stop bleeding. The leukaemia is stopping all of these blood cells from being made. This is really dangerous as your immune system can’t work any more, and any infection is dangerous. You are at risk of bleeding. The leukaemia cells cram up your blood vessels and they can block them off which would cause painful areas to appear.
Nods slowly.
Did they give you a timeframe?
Shrug.
Would you like me to talk about your time frame?
Nod.
I’m not sure how much time you have left. It could possibly be only days to short weeks. Things could worsen quickly and then you might only have hours to days left.
Oh.
We want you to know that we are prepared for what usually might occur in your kind of situation. If you need emergency treatments we want them to be available at any time.
Nod.
I’m sorry to have to give you bad news. If you still have important things you need to sort out, it’s better to do it now while you are still clear in the head. Better early than too late.
Points to his computer. That’s what I’m doing.
Good. What’s the most important thing to you right now?
Points to his partner. She wraps her arms around his head and cries into his hair. He clutches her arm tightly and cries into her forearm. They hold each other tight and sob loudly.
Let it all out. It needs to come out. You are safe here. We are all here to help you. We will get you through this, both of you.









