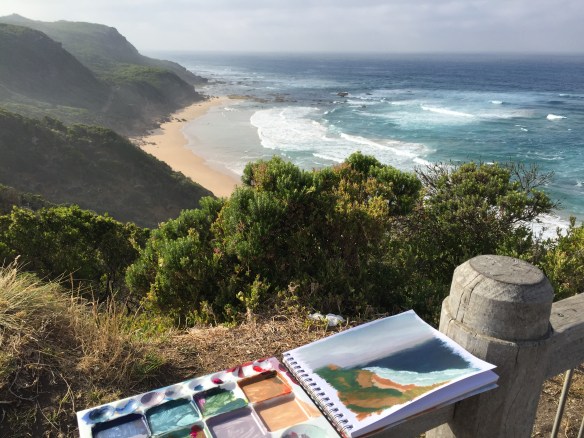
Photo by Miran Rijavec via flickr
Dr David Brumley is a palliative care specialist with extensive experience working in regional Victoria and across South East Asia. Here he reflects on the importance of spirituality and self care in palliative care practice.
Dr Doug Bridge ran a Spirituality Workshop last September in Melbourne, as part of the 2015 Palliative Care Australia conference. To my knowledge this was the first such workshop associated with a palliative care conference – in Australia, at least. Unsurprisingly, it was very well received. Thanks Doug.
The existence of Spirit and the possibility of spiritual distress and suffering seems unarguable. If spirituality is the ground of our being, spiritual suffering could be seen as our alienation from that. With variations, many definitions observe the four aspects of spirituality to include relationship with self, others, environment and the transcendent. Such descriptions might allow acceptance by both the religious and atheist. The literature refers to many ways to measure these aspects of spirituality. For example, John Fisher developed SHALOM, a questionnaire that examines these four areas. We applied this questionnaire to members of the Australian and New Zealand Society of Palliative Medicine (ANZSPM) in 2007-8. Many surveyed doctors didn’t feel they had the capacity to help patients in the domains of spirit.
Dying people suffer spiritual distress, and doctors might sometimes be best placed to identify and provide, at the least, initial help. Our own spiritual wellbeing is also needed if we are to care for them and for ourselves and avoid personal distress and injury. The spiritual health of the patients we care for is our responsibility. So is our own. I wonder if they are two sides of the same coin? Ralph Waldo Emerson thought so: “It is one of the most beautiful compensations of this life that no man can sincerely try to help another without helping himself.”
Doctors need to be able to recognise and at least provide initial care of spiritual distress. Do we know what it looks like? Where are the boundaries between psychology and spirituality? How does a doctor approach the question of spiritual assessment of a patient? How would a model of spiritual care be different, for example, from existential psychotherapy? How might it be useful? What are the required skills for such care? What should we take on, and when and to whom should we make referrals? I don’t think we have developed adequate answers to these questions.
Should a structured approach to self-care include a spiritual component? What advantage would that have for us? Should our College have something to say to trainees about spiritual care of others and ourselves? The Royal College of Psychiatrists believes so, but not everybody. A recent Twitteration on the issue of mindfulness in schools in the USA suggested that many people believed that meditation is inherently a practice of other religions. Don’t look inside, for goodness sake!
As a group we know we must be high-level communicators. Should we also aim for an overt training in talking about what life means, even if it is about to cease, or should we simply follow Osler, and “minister to our patients through warm human contact”? Is that enough? I don’t think so.