Our patient was reviewed by the surgeon in our inpatient unit. It was kind of the doctor to see him at our hospice. Our patient and his wife were able to discuss everything with the surgeon and he left them to think about the proposed operation. They talked about this with a number of our staff and then discussed it with me. We went through all the possible benefits and risks and we decided together that they would like to try the operation.
The operation would involve removing a specific part of the spinal cord in order to disrupt the nerve pain from being transmitted.
The operation went as planned and our patient recovered well from it.
We were expecting him to come back to our inpatient unit for a period of rehabilitation but he was good enough to go directly home.
The operation had successfully controlled his nerve pain, and we could reduce his medications a lot.
He was well enough to go to his holiday home for some weeks in the summer, something he had thought he’d never be able to do again.
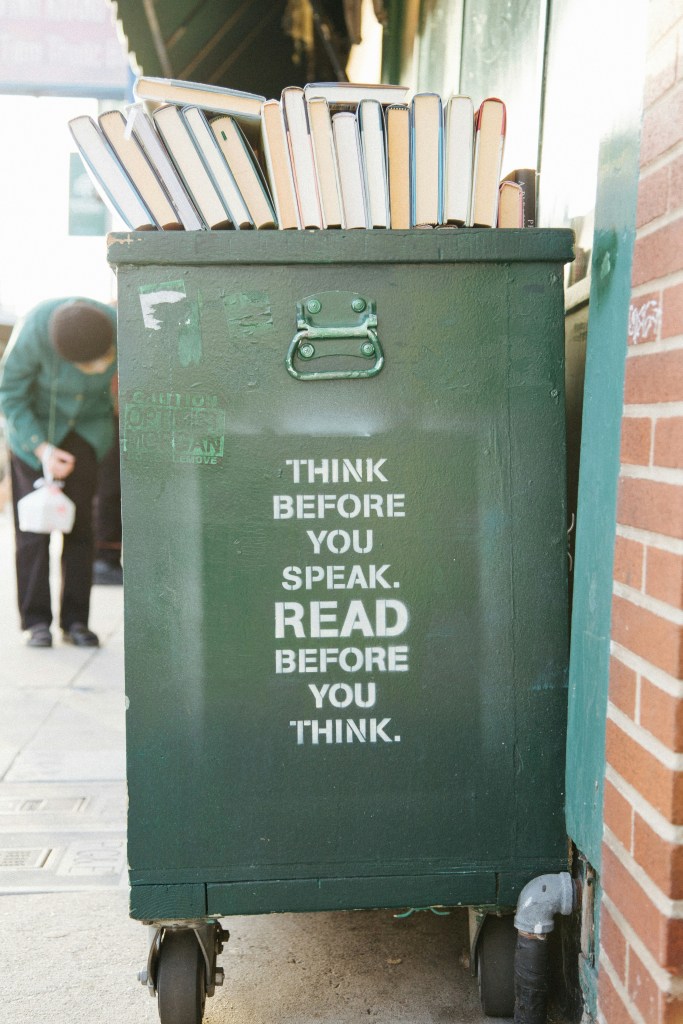
Physically his pain was well controlled but the non-physical aspects of his pain remained. The existential and emotional distress were not improved at all, in fact they might have worsened. A common side effect of the pain relief medications he had used was drowsiness. Now that he didn’t need as much physical pain medication he was less sleepy, and had more time to think. More time to think about the grimness of his reality.
Unfortunately our proud patient had refused all input from mental health services or counselling. The idea of talking to people about his feelings was an alien concept for this self-described working class man. He just couldn’t discuss these things with anyone, it was a step that would always be too far for him to ever take.
I was called by the staff of the local hospice which covered the area where his holiday house was. They had been asked to call me for my opinion on what they should do in regards to further treatments of life-threatening infection. Knowing the man as well as I did, I didn’t think further treatments would be helpful. He was miserable and staying alive longer to be more miserable would not help him and would only prolong his suffering.
Psychologically he continued to shut down and withdrew from the world. He died at home after being well looked after by his devoted wife with the assistance of our visiting staff members.