How much time has she got left doctor?
She likely only has days left to live.
Days?!
Yes, probably just days.
Really?
Yes, it could actually be much shorter if she deteriorates faster.
Thanks. We have things we need to prepare.
No matter how long she has got left we will do our best to keep her comfortable.
Thank you.
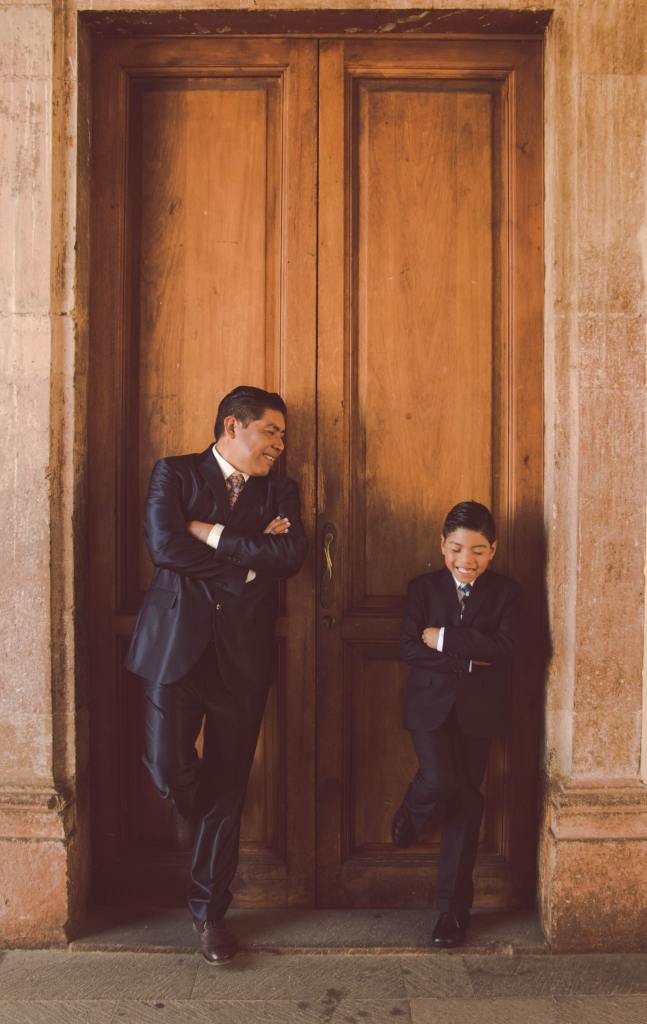
She’s been an important part of you and your children’s lives.
Yes. It’s hard, it’s the first time we’ve been through something like this.
We’re going to get your mother through this, we’re going to get you all through this. If you have any worries or concerns please share them with us. Our job is to take as much stress out of this situation as possible. Please let us know if there is anything we can help you with.
Thank you. We brought you some cakes.
You brought three cakes, that’s very generous of you.
Yes, one for each of the nursing shifts.
That’s nice of you to think of each of the shifts.
The staff have looked after us all well. Thank you.
That’s what we are here for. We’ll see you later, try and get some rest when you can. Thanks again for the cakes.
You’re welcome, see you later.