He loved to work. He said it made him happy. He said it took his mind away from what he was going through with his illness. The doctor had given him bad news. Time was going to be short, possibly only weeks left to live. He still wanted to work, he had asked his boss to bring in a laptop, and other work equipment. He said he wouldn’t do too much work, and that if he was too tired he would stop.
His wife looked doubtful and talked about trying to spend all her time with him, but he chose to work even when she was there. This was something that she couldn’t bear to watch. It had happened too often. She wanted me to tell him to stop working. I couldn’t tell this dying man not to do something that would make him happy. I tried to negotiate a compromise between them.
“I’m not here to tell you what to do. You’ve been told you might only have weeks left to live. How you use your time is up to you. I can’t make those decisions for you. You need to think about how you want to spend whatever time and energy you have left. I’m here to take away whatever stress I can. I don’t want you two arguing at this stage of your relationship. Why don’t we try to balance things out more? Your wife needs to take a break, maybe go home for a few hours a day. Why don’t you work when she has gone out? When she comes back, then it’s time to stop working. Do you both think that will work? My staff and I will keep an eye on you, we don’t want you overdoing it, and if it looks like you are exhausting yourself we will tell you to work less. Thank you both for agreeing to try this out. I will be checking in with you both, to see how much breaks/work you both have/do.”
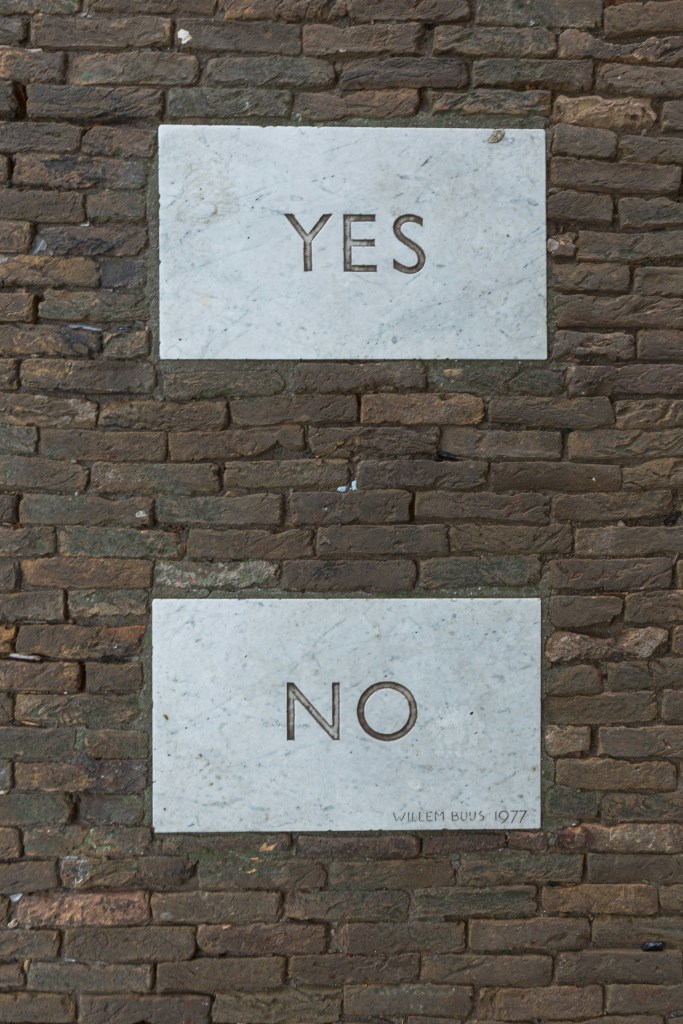
I wasn’t sure how well it would go. It is hard not to be yourself after a lifetime of being in the role. People stay true to themselves right to the end. That being said just in the past days he had agreed to be baptised into his wife’s life-long religion. A huge change for a man who had been an atheist over his adulthood. I would try to keep an open mind and see what happened next.