I went to see the new patient who had just arrived by ambulance. A Chinese man in his 30s who was drowsy and confused. He wasn’t able to move out of bed, and needed full assistance with all cares. He was accompanied by his wife and his father. Our patient’s English was reported as good but he wasn’t alert enough to answer many questions.
“Where are you sore?”
Hands pointed to his abdomen as he grimaced.
His father said, “He’s always considered other people before himself. That’s how he’s been since he was a young boy.”
I made some adjustments to the patient’s medication to try to ease the suffering.
His father came to speak to me, and I ushered him into a small meeting room.
He was angry and devastated. He spoke to me in Cantonese which I have some understanding of, thanks to a childhood of watching Hong Kong TV series on VHS video tapes. My usual slow process with Cantonese, is to convert it into Mandarin and then into English. I have trouble when trying to go back the other way, so don’t speak Cantonese.
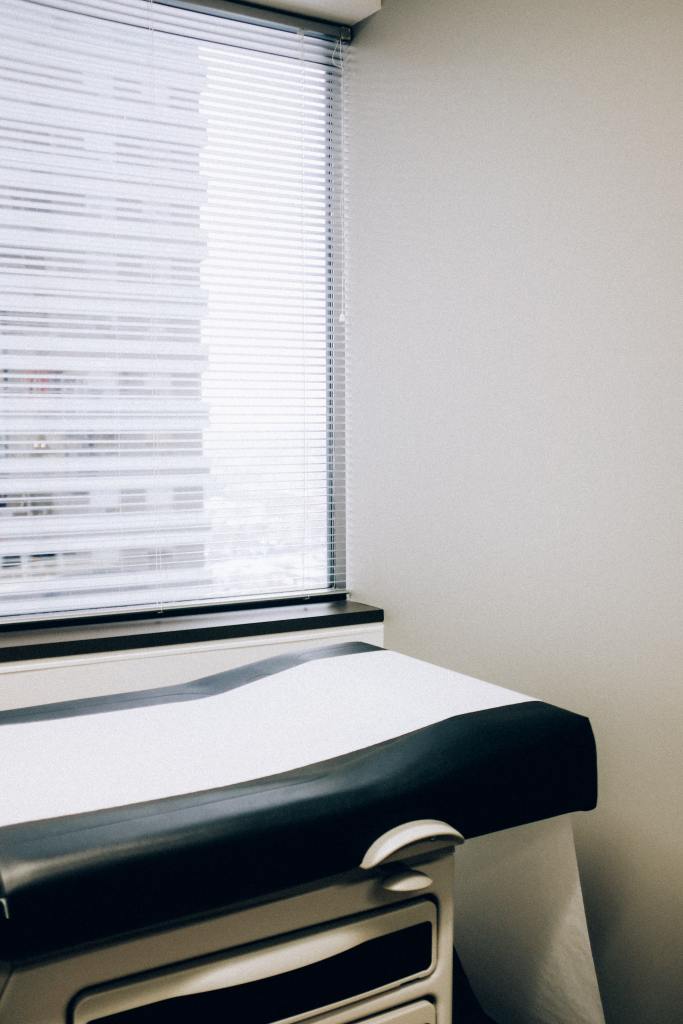
He recounted the clinic appointment they had attended yesterday. They had driven from home to the Oncology Centre. His son required a wheelchair as he could not walk the long distances. The Oncology registrar that met them was Chinese and spoke Cantonese. He asked if his son could lie on the bed as he was tired from sitting up for hours to get to clinic. The registrar answered no, that the clinic was too busy today. This surprised the father who said, “Couldn’t they see how unwell he was? Then they told us bluntly, there was nothing they could do for my son. That he was dying. I was so angry that I wanted to complain, but my son wouldn’t let me, he told me to leave it, and that he wanted to go home.” I listened to him for 45 minutes and talked to him in Mandarin which was our shared second language. He had calmed down and was able to head back into his son’s room.
Continue reading








