
Albany wind farm
This post is a year overdue. If I were to have written this in April 2015, the title would have been “The tale of two deaths” where I would have reflected upon the peaceful, managed and expected passing of a 93-year-old aged care patient contrasted with the tragic accidental death of a 19-year-old patient whom I’d seen only a week earlier.
But what I’ve learnt is that tragic accidents are random, unexpected and do not happen often. More importantly I have been involved in the end-of life care of several patients since then, that have taught me a great deal about palliative care medicine, the value of open and frank conversations with family and some of the myths surrounding the management of death.
This is also a story of my maturity through being stretched and learning that the part of medicine that I ran away from the most has ended up becoming my greatest passion and future, aged and palliative care.
As a young hospital doctor, I was into the high fives and exhilaration of acute care medicine. I dreaded being the doctor in the emergency department who picked up the older patient from a nursing home because I didn’t really know how to approach their issues.
This bias continued into my general practice training but I was then persuaded to assume the care of 6 aged care patients from a retiring GP, I was confronted again!
I Initially refused for a few months but then started to receive faxes addressed to Dr. Ramachenderan! Well my fate was sealed and I started to visit these patients every month and interact with their families and this started to make a strong impression on me.
Many of these patients just wanted me to sit next to them and talk, hold their hand and just be. I would solve problems such as urinary tract infections, agitation, pain and inevitably I would learn about managing symptoms of their decline and eventual passing.
“One of the greatest lessons in medicine and life, is that you will never grow unless you are pushed outside your comfort zone. Outside the comfort zone is where you expand your knowledge, accelerate your growth and hopefully become wiser. Outside the comfort zone is where all people should strive to be, because inside is ordinary, garden variety, homogenous and boring! Ask yourself where do you want to be?” – Dr. Jonathan Ramachenderan
My first death was far outside my comfort zone and my training that I received as a GP.
I was urgently called to see Eunice (not her real name), who was a 90-year-old spinster who had been a seamstress for most of her life and had a background of Alzheimer’s disease, chronic renal failure and previous breast cancer. As I approached her bedside, her frail body was covered delicately with her favourite rug, her breathing was rapid and she was unsettled, appearing to be in distress.
During her decline in the previous weeks, she had fallen numerous times as she weakened, X-ray’s were normal but then she started to cough and vomit bilious liquid. With her advanced dementia, she couldn’t understand why she wasn’t able to walk and became agitated and sometimes aggressive.
I was out of options, I knew she was dying and in pain but wasn’t quite sure how to approach these issues.
Needless to say, our Great Southern Palliative care team visited her several times and helped guide me with her medications to ease her agitation and anxiety, settle her nausea and relieve her pain.
As her symptoms settled, she gradually stopped climbing out of bed and she was able to sit peacefully in her chair, bathing in the filtered rays of the sun.
Then one day, a few weeks later, I received a call from the nursing home early in the morning letting me know that Eunice had passed away in her sleep. Inside I felt a mixture of relief that she wasn’t being troubled by her symptoms anymore but also sadness because I had visited her several times in the last few months, talked to her family openly about her trajectory and wishes and I had unexpectedly grown close to her.
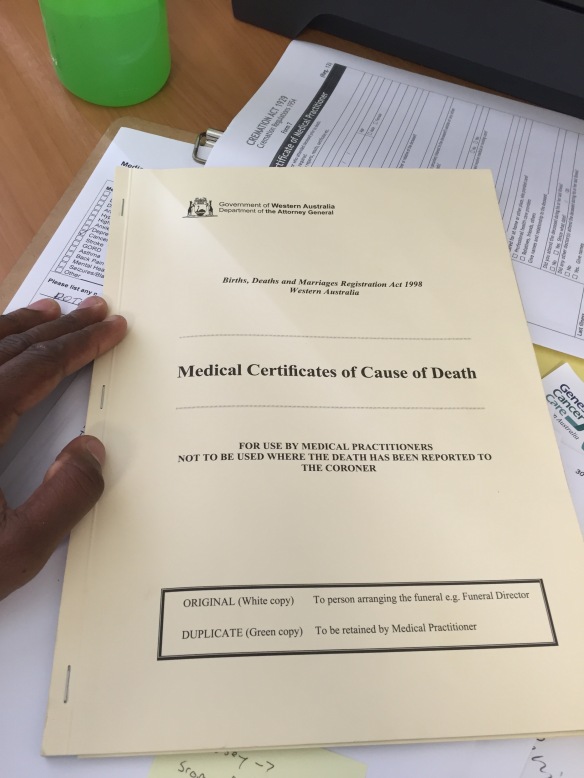
Little did I know that this experience was preparation for my future as an aged care GP, because since Eunice’s passing I have been involved in the end-of life care of several of my aged care patients. Recently I made our administration staff laugh nervously when I suggested that I should keep the death certificate book in my bag! But it has been this way over the last few months.
Each of these patients has had an impact on my life because they allowed me into their world as I visited their room every few weeks, listened to stories about their family, laughed at their jokes, rejoiced in their good news and also been the bearer of bad news.
Taking care of patients at the end of their life has deeply humbled me and left me embarrassed about my initial immature attitude. But salvation has come in the families who have sincerely thanked me, shared a tear with me and the peaceful and respectful way that their loved ones have passed away.
There is still a great deal to learn but the one thing I know, is that by giving my patient’s a voice through respecting their wishes, relieving their symptoms so that they can continue their journey and providing an opportunity for their families to talk openly, I believe that I am on the right track.
This is my unexpected journey into aged and palliative care, a place where I was meant to travel to.

Dr. Jonathan Ramachenderan is Rural Generalist from Albany, Western Australia. He has a growing interest in palliative care medicine which has developed from his aged care and general practice work. He blogs about marriage, parenting and living a larger life at his blog www.thehealthygp.com
Photos supplied by Dr Ramachenderan

Reblogged this on The healthy GP and commented:
Thank you to my friends at Palliverse for graciously offering me a platform to share the first in many stories and articles about my journey into aged and palliative care.
Please look into http://palliverse.com and follow them on twitter @palliverse
LikeLike
Hi Jonathan,
I, too, am a GP with a strong interest on Aged Care and Palliative Care, and I also derive a great deal of enjoyment and professional satisfaction with caring for my older patients. As a GP, I often cared for them in the community before their health declined and they needed to enter the RACF. So, the connection was there, and many are pleased to learn that I would still be visiting them.
One of the joys over my professional life-time (over 25 years!) is how the focus of many RACFs and their staff has changed in helping to manage their patients. I find that there is less of a reliance on medication and more on environmental strategies. There is still a lot of room for improvement, but I think back to 1990 and then to now, and there has been a huge improvement in the built environment and the caring environment in that time.
Sadly, care within RACFs is under-researched and that is something that I would like to see improved, but I am never sure how to start.
Thank you for sharing your story. I really enjoyed your honesty and empathy.
LikeLiked by 1 person
Thank you for taking the time to read this piece!
I didn’t think I’d be here talking about aged and palliative the way that I am now, mainly because to arises from a place deeper than many of the superficialities of the world
Isn’t it so greatly rewarding to care for your patients from the community as they age and allow them to respectfully enjoy the last days of their life in comfort and peace?
We are quite interested in ACF research as I am very blessed to work with a team of nurses with an academic background. One of the first projects that we would like to undertake is actually about carer and nurses burnout and whether interventions such as regular debriefing and short wellbeing/stress management presentations can have an impact on this.
Its a start but I think being able to care for the carers and nurses is one the biggest ways we can stop turnover within the industry but also make aged care an attractive place for our best and brightest to lead and innovate.
I really appreciate your encouragement and sharing your experience, I am keen to connect and learn more!
Sincerely
Jonathan
LikeLike
Are you a member of ANZSPM? I am going to the conference in Perth later this year.
LikeLike
I think might, after all its in WA! the GP looks very interesting.
LikeLike
Hi Jonathon – how wonderful to read this piece all the way from where I am sitting in Cambridge. I look forward to getting back home and working alongside you and the rest of the Palliative Care team. It’s interesting how similar my own experience of coming from what I thought was my chosen path (of ED), via an unplanned RMO term in Cottage Hospice, into Palliative Care, has made my working and whole life so much richer.
LikeLiked by 1 person
Dear Kirsten, thank you for taking the time read this piece and comment, I am honoured!
Discovering a passion that fits into your natural gifts and abilities as a person is where we do our best work. That is why we are all so very blessed to have you in Albany to help lead and teach us.
Enjoy your time making memories and will see you when you are back! Thank you Kirsten.
LikeLike